Last updated July 17, 2017 at 11:26 am
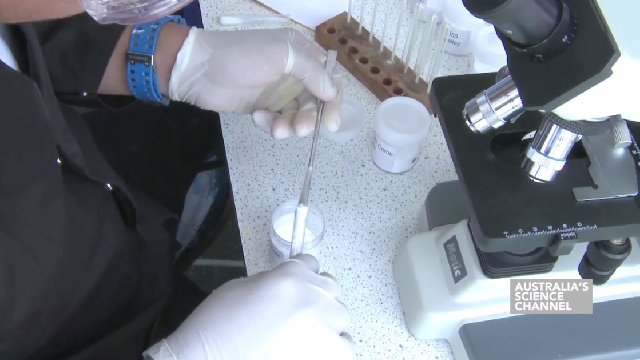
There’s no time like now to fight superbugs. Researchers have developed a new way to measure antibiotic tolerance, which might give doctors a better way to prescribe antibiotic treatments.
 Researchers have now developed a new method that measures antibiotic tolerance, the time it takes to kill bacteria that have become tolerant to antibiotic drugs, as published in The Biophysical Journal.
Researchers have now developed a new method that measures antibiotic tolerance, the time it takes to kill bacteria that have become tolerant to antibiotic drugs, as published in The Biophysical Journal.
One of the biggest threats to human healthcare is the build-up of antibiotic resistance. Part of understanding this includes antibiotic tolerance which is often associated with treatment failure and relapse. It’s seen as the stepping stone towards antibiotic resistance.
The researchers hope that this new method will be used in the clinical setting to help doctors determine the length of time required for antibiotic treatment. Determining the dose and duration of antibiotic treatments is a tightrope that doctors must balance on. If you under-treat, more resistant bacteria in a patient could survive and increase the chance of the patient getting sick again. If you over-treat, there could be side effects in the patient as well as the waste of the antibiotics themselves. Current methods are based on the minimum drug concentration required to prevent bacterial growth, known as the minimum inhibitory concentration (MIC). This is a measurement of antibiotic resistance.
Antibiotic tolerance is very different from antibiotic resistance. “Tolerance is an extension of the period of time that bacteria can survive in lethal concentrations of an antibiotic (many times the MIC) before succumbing to its effects”, as the researchers explain in their research paper.
So again, because death is not instantaneous, there’s the question of how long does it take to kill bacteria.
To determine this, the researchers developed a metric called the minimum duration for killing 99% of the population (MDK99). They demonstrated this with six strains of E. coli with ampicillin, a common antibiotic treatment, and found varying tolerance levels from 2 to 23 hours. They shared their method so that others can also do this themselves.
“A take-home message from this is that it is important to complete a course of antibiotic treatment as prescribed, even after the disappearance of the symptoms,” senior study author Nathalie Balaban says.
Not only will these new findings possibly help doctors but they hope they can be used experimentally to study the evolution of tolerance in patients. This is just another way that researchers are trying to win the leap-frog game between antibiotics and superbugs.
- Link to original research article: cell.com/biophysj/fulltext/S0006-3495(17)30551-9
Follow us on Facebook, Twitter and Instagram to get all the latest science.